Introduction
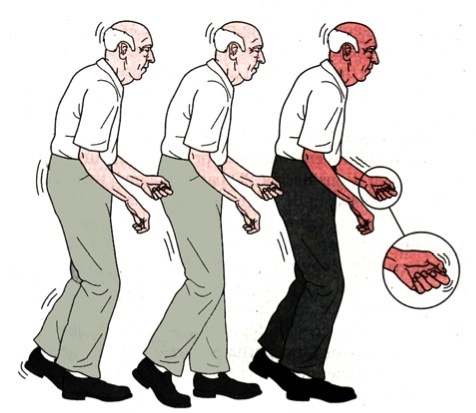
Parkinson’s disease is a degenerative disorder of a central nervous system. The early symptoms included but are not limited to shaking, rigidity, slowness of the general movements, and difficulty in walking, cognitive and behavioural problems which normally occurs in the advanced stages.
Currently, this is affecting almost 1% of the population aged 65 and above. This is a fourth most common neurological disorder affecting elderly. The disease has an insidious onset and is slowly progressive leading to severe morbidity in advanced age.
Causes
Idiopathic
Most people with Parkinson’s disease have idiopathic Parkinson’s disease (having no specific known cause).
Genetic factors
Generally, Parkinson’s disease is considered to be a non-genetic disorder
Around 15% of individuals with PD have a 1st-degree relative who has the disease
5% (approximately) people are known to have Parkinson’s disease that occurs because of a mutation of one of the several specific genes. The most extensively studied PD-related genes are SNCA and LRRK2.
Several Parkinson-related genes are involved in the function of lysosomes, organelles that digest cellular waste products. Some forms of Parkinson’s disease may be caused by lysosome dysfunctions that reduce the ability of the cells to break down alpha-synuclein.
Other factors
These have been associated with the risk of developing PD, but no causal relationship has been proven.
- Accelerated ageing
- Environmental toxins (methyl-phenyl tetra hydro pyridine- MPTP) and other toxins (manganese, carbon monoxide, and methanol)
- Increased free radical and iron content in the Substantia Nigra
- Drugs – Reserpine, Ethanol, Lithium, Diltiazem etc.
- Neurodegenerative disorders such as multi-system atrophy, Alzheimer’s disease
- Post infections (viral encephalitis etc.)
- Brain tumor
- Repeated head injury
Pathology
Lewy bodies are a key pathological feature of Parkinson’s disease.
Anatomical:
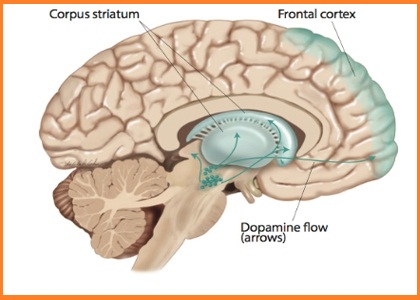
Basal ganglia are a group of brain structures. They are innervated by the dopaminergic system. These areas are highly affected in Parkinson’s disease.
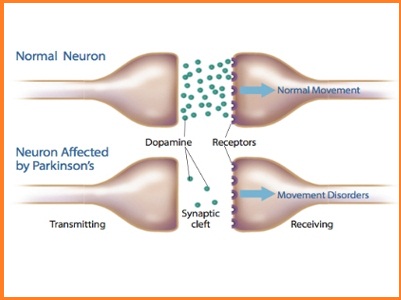
The main pathological characteristic of PD is cell death in the substantia nigra and more specifically, the ventral (front) part of the pars compacta affecting up to 70% of the cells by the time death occurs.
Macroscopic:
Reduction of neuromelanin pigmentation in the substantia nigra and locus coeruleus suggests neuronal loss on cut surfaces of the brainstem.
Microscopic (histopathology):
Neuronal loss in the substantia nigra and several other brain regions and Lewy Bodies in many of the remaining nerve cells.
Neuronal loss is accompanied by the death of astrocytes (star-shaped glial cells) and activation of the microglia (another type of glial cell).
Classification of Parkinson’s disease
Parkinsonism or Parkinsonian Syndrome is a term used to describe the collective motor symptoms of PD.
Parkinsonian syndromes can be divided into four subtypes according to their origin:
- Primary or idiopathic
- Secondary or acquired,
- Hereditary Parkinsonism
- Parkinson-plus syndromes or multiple system degenerations
- Primary or idiopathic Parkinsonism:
It is the name given for Parkinson’s disease which is the most common form of Parkinsonism
This type of Parkinsonism does not have any external identifiable cause
Genetic Parkinson’s disease’s with a similar clinical course to PD are generally included under this type.
- Secondary or acquired Parkinsonism:
This manifests as a result of some other disorder
- Hereditary Parkinsonism:
Off late, many genes that are directly related to some cases of PD have been discovered. The terms ‘Familial Parkinson’s disease’ and ‘Sporadic Parkinson’s Disease’ are used to differentiate genetic types of PD from truly idiopathic forms of PD
- Parkinson-plus syndromes or multiple system degenerations:
Other than causing movement related disorders, PD also gives rise to several non-motor types of symptoms such as sensory deficits, cognitive difficulties or sleep problems. Parkinson-plus diseases are Primary Parkinsonisms with additional features. They include – multiple system atrophy, progressive, supranuclear palsy, corticobasal degeneration and dementia with Lewy bodies.
Signs and symptoms
Primary symptoms:
Four motor symptoms are considered cardinal in PD:
- Tremor
- Rigidity
- the slowness of movement
- postural instability
The primary symptoms of Parkinson’s disease are all related to voluntary and involuntary motor function and usually start on one side of the body.
Symptoms are mild at first and will progress over time. Some individuals are more affected than others. Studies have shown that by the time that primary symptoms appear, individuals with Parkinson’s disease will have lost 60% to 80% or more of the dopamine-producing cells in the brain.
Characteristic motor symptoms include the following:
Tremors: Trembling in fingers, hands, arms, feet, legs, jaw, or head. Tremors most often occur while the individual is resting, but not while involved in a task. Tremors may worsen when an individual is excited, tired, or stressed.
Rigidity: Stiffness of the limbs and trunk, which may increase during movement. Rigidity may produce muscle aches and pain. Loss of fine hand movements can lead to cramped handwriting (micrographia) and may make eating difficult.
Bradykinesia: Slowness of voluntary movement. Over time, it may become difficult to initiate movement and to complete the movement. Bradykinesia together with stiffness can also affect the facial muscles and result in an expressionless, “mask-like” appearance.
Postural instability: Impaired or lost reflexes can make it difficult to adjust posture to maintain balance. Postural instability may lead to falls.
Parkinsonian gait: Individuals with more progressive Parkinson’s disease develop a distinctive shuffling walk with a stooped position and a diminished or absent arm swing. It may become difficult to start walking and to make turns. Individuals may freeze in mid-stride and appear to fall forward while walking.
Secondary symptoms
While the main symptoms of Parkinson’s disease are movement-related, progressive loss of muscle control and continued damage to the brain can lead to secondary symptoms.
Some of the secondary symptoms include:
- Anxiety, insecurity, and stress depression, confusion, memory loss and dementia (more common in elderly individuals)
- Executive dysfunction, Slowed cognitive speed
- Insomnia, daytime drowsiness, mask-like face expression
- Small handwriting, quieter speech, and monotone voice. Difficulty in speech, swallowing and excessive salivation
- pain, paresthesia, Fatigue, Dystonia (abnormal, sustained, painful twisting muscle contractions)
- excessive sweating
- Altered sexual function
- skin problems, oily skin
- urinary incontinence
- Constipation
- diminished sense of smell (hyposmia or anosmia)
- blurred or double vision, decreased blink rate, dry eyes
- Psychotic symptoms—hallucinations or delusions
- low blood pressure upon standing (orthostatic hypotension)
Diagnosis
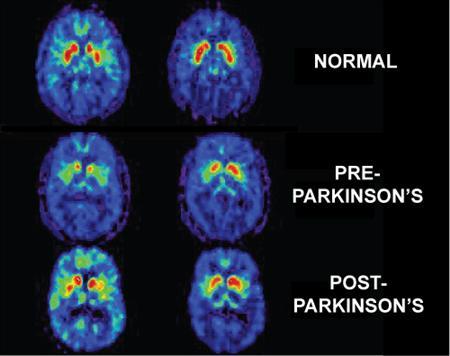
An early and accurate diagnosis of Parkinson’s disease is important in developing good treatment strategies to maintain a high quality of life for as long as possible. A physician will diagnose Parkinson’s disease from the medical history and a neurological examination. There is no lab test that will clearly identify the disease, but brain scans and other laboratory tests are sometimes used to rule out disorders that could give rise to similar symptoms.
Other causes that can produce secondary PD are:
- Alzheimer’s disease
- Multiple cerebral infarction
- Drug-induced Parkinsonism
- Parkinsonism plus syndromes – such as Progressive supranuclear palsy & multiple system atrophy should be ruled out (anti-PD medicines are less effective in these syndromes)
Patients may be given levodopa and resulting relief of motor impairment tends to confirm the diagnosis.
Individuals may sometimes be misdiagnosed as having another disorder, and sometimes individuals with Parkinson-like symptoms may be inaccurately diagnosed as having Parkinson’s disease.
It is, therefore important to re-evaluate individuals in the early phase on a regular basis to rule out other conditions that may be responsible for the symptoms.
Differential Diagnosis
- Drug-induced Parkinson
- Depression
- Essential tremor
- Normal pressure hydrocephalus
- Cerebral hypoxia
- Carbon monoxide poisoning
Medical Pathology
Medical research has determined the cause of the condition to be a loss of function of specialized cells in the brain stem which stimulate the production of the neurotransmitter, dopamine 9,1. The cause of the functional disturbance is not known. It is known that Parkinson’s disease can occur secondarily to several known causes, including the ingestion of anti-psychotic drugs such as reserpine. These drugs block the action of dopamine on the brain even though normal levels are present. In addition, carbon monoxide and manganese poisoning can instigate the condition, as well as other brain tissue abnormalities such as tumors and infarcts.
Investigations
There are no confirmatory tests available; diagnosis is commonly made on clinical grounds. The following investigations may help in the diagnosis.
- CT Scan
- MRI Scan
- Positron-Emission Tomography (PET)
- Levodopa drug challenge test